Introduction: When Restless Nights Become a Pattern
We’ve all had the occasional sleepless night — tossing and turning before a big presentation or waking up at 3 a.m. worrying about tomorrow’s to-do list. But for millions of people, poor sleep isn’t just an occasional inconvenience — it’s a chronic struggle tied to a sleep disorder. According to the American Sleep Association, nearly 70 million U.S. adults suffer from some form of sleep disorder. Left untreated, these conditions can affect everything from memory and mood to heart health and immune function.
The good news? Most sleep disorders are both recognizable and treatable. By learning the signs, understanding the risks, and exploring science-backed solutions, you can take meaningful steps toward more restful nights.
Understanding Sleep Disorders: Why They Matter
Sleep is more than “down time.” While you sleep, your body repairs tissues, balances hormones, consolidates memories, and even detoxifies the brain. Chronic disruptions in this process increase the risk of:
-
Cardiovascular disease
-
Type 2 diabetes
-
Anxiety and depression
-
Memory decline
-
Weakened immunity
Recognizing sleep disorders early can prevent these long-term consequences and restore both energy and health.
The Most Common Sleep Disorders
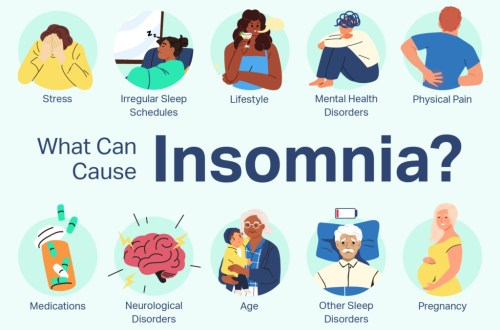
1. Insomnia
What it is: Difficulty falling asleep, staying asleep, or waking too early.
Signs: Lying awake for more than 30 minutes, waking frequently at night, daytime fatigue, irritability.
Causes: Stress, anxiety, poor sleep hygiene, medications, or underlying health conditions.
Solutions:
-
Create a consistent bedtime routine (same sleep/wake time daily).
-
Limit caffeine and alcohol, especially in the evening.
-
Use relaxation techniques like deep breathing or meditation before bed.
-
Consider Cognitive Behavioral Therapy for Insomnia (CBT-I), a proven non-drug treatment.
2. Sleep Apnea
What it is: A disorder where breathing repeatedly stops and starts during sleep.
Signs: Loud snoring, choking/gasping during sleep, morning headaches, excessive daytime sleepiness.
Risks: High blood pressure, stroke, heart disease, and memory problems.
Solutions:
-
Get evaluated with a sleep study (at-home or in-lab).
-
Use CPAP therapy (Continuous Positive Airway Pressure) if prescribed.
-
Lose excess weight and avoid alcohol before bedtime.
-
In some cases, oral appliances or surgery may be recommended.
3. Restless Legs Syndrome (RLS)
What it is: An uncontrollable urge to move your legs, often worse at night.
Signs: Tingling, crawling, or “pins and needles” sensations that improve with movement.
Causes: Sometimes linked to iron deficiency, pregnancy, or chronic conditions like kidney disease.
Solutions:
-
Stretching and light exercise in the evening.
-
Reducing caffeine and alcohol.
-
Checking with your doctor about iron levels or medications that may worsen symptoms.
-
Prescription medications (like dopamine agonists) if lifestyle changes aren’t enough.
4. Narcolepsy
What it is: A neurological disorder that affects the brain’s ability to regulate sleep-wake cycles.
Signs: Excessive daytime sleepiness, sudden loss of muscle tone (cataplexy), sleep paralysis, vivid hallucinations at sleep onset.
Impact: Narcolepsy can interfere with work, school, and safety (especially driving).
Solutions:
-
Scheduled naps during the day.
-
Medications that promote alertness or regulate REM sleep.
-
Avoiding alcohol and heavy meals before important tasks.
-
Creating a consistent daily routine.
5. Circadian Rhythm Disorders
What it is: A mismatch between your internal body clock and your external environment.
Examples:
-
Delayed Sleep Phase Syndrome (night owls who can’t fall asleep until very late).
-
Shift Work Disorder (irregular schedules disrupt sleep).
Signs: Trouble falling asleep/waking at socially acceptable times, daytime grogginess, reduced focus.
Solutions:
-
Exposure to natural light in the morning to reset the body clock.
-
Using blue-light blocking glasses at night.
-
Sticking to a sleep schedule, even on weekends.
-
Strategic use of melatonin (under medical guidance).
Practical Steps You Can Try Tonight
Improving sleep doesn’t always require medication. Here are simple, science-backed habits you can implement right away:
-
Set a consistent bedtime. Your body thrives on routine.
-
Create a wind-down ritual. Try reading, journaling, or gentle stretching.
-
Cool, dark, quiet. Keep your room around 65–68°F, use blackout curtains, and reduce noise.
-
Limit screens before bed. Blue light suppresses melatonin, delaying sleep.
-
Mind your meals. Avoid heavy dinners and late caffeine.
-
Move your body. Regular exercise (but not right before bed) improves sleep quality.
If these don’t help and symptoms persist, it’s time to seek a professional sleep evaluation.
When to See a Doctor
You should consider talking to a sleep specialist if:
-
You regularly sleep less than 6 hours despite trying lifestyle changes.

-
You snore loudly, gasp, or stop breathing during sleep.
-
You feel excessively tired during the day, no matter how much you sleep.
-
Uncomfortable leg sensations keep you awake at night.
A doctor may recommend a sleep study (polysomnography) to diagnose conditions like sleep apnea or narcolepsy.
Conclusion: Better Sleep Is Possible
From insomnia to sleep apnea, sleep disorders can feel overwhelming — but they don’t have to control your life. With the right awareness, lifestyle changes, and medical support, restful nights and refreshed mornings are within reach.
Sleep isn’t just about feeling less tired — it’s about protecting your heart, mind, and long-term health. If your nights are restless and your days are dragging, take action today. A healthier, more energized version of you is waiting on the other side of a good night’s sleep.