Introduction: More Than Just Being Tired
 Everyone feels sleepy now and then — whether it’s from staying up too late or powering through a busy week. But for people with narcolepsy, daytime sleepiness isn’t a choice, it’s a constant struggle. Narcolepsy is a neurological sleep disorder that affects the brain’s ability to regulate sleep-wake cycles, leading to overwhelming fatigue and sudden sleep attacks that can happen anytime, anywhere.
Everyone feels sleepy now and then — whether it’s from staying up too late or powering through a busy week. But for people with narcolepsy, daytime sleepiness isn’t a choice, it’s a constant struggle. Narcolepsy is a neurological sleep disorder that affects the brain’s ability to regulate sleep-wake cycles, leading to overwhelming fatigue and sudden sleep attacks that can happen anytime, anywhere.
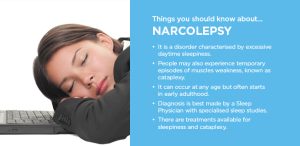
This condition may sound rare, but it impacts an estimated 1 in 2,000 people worldwide — and many go undiagnosed. Understanding narcolepsy is the first step toward finding relief and improving quality of life.
What Is Narcolepsy?
Narcolepsy is a chronic neurological disorder that disrupts the way your brain manages sleep and wakefulness. Unlike normal sleep, which progresses through stages gradually, narcolepsy can cause people to enter REM sleep almost immediately — even during the day.
There are two main types:
Narcolepsy Type 1 (NT1): Includes excessive daytime sleepiness and cataplexy (sudden loss of muscle tone).
Narcolepsy Type 2 (NT2): Involves daytime sleepiness without cataplexy.
Symptoms to Watch For
Narcolepsy symptoms often begin in adolescence or early adulthood and may worsen over time. The four classic signs include:
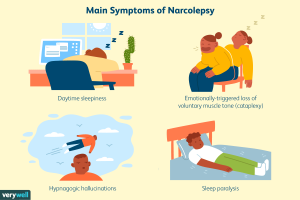
Excessive Daytime Sleepiness (EDS)
Feeling persistently tired, regardless of how much sleep you get.
Falling asleep suddenly during work, school, or even conversations.
Cataplexy (Type 1 Narcolepsy)
Sudden muscle weakness triggered by emotions like laughter, surprise, or anger.
May cause slurred speech, knee buckling, or even collapsing.
Sleep Paralysis
A frightening inability to move or speak while falling asleep or waking up.
Often accompanied by a feeling of being “pinned down.”
Hallucinations
Vivid, dreamlike visions that occur when falling asleep or waking.
Can feel so real that they cause anxiety or confusion.
What Causes Narcolepsy?
The exact cause isn’t fully understood, but research points to a loss of hypocretin (orexin) — a brain chemical that helps regulate wakefulness and REM sleep. Potential triggers include:
Autoimmune response: The immune system mistakenly attacks hypocretin-producing brain cells.
Genetics: Certain genes increase susceptibility.
Brain injury or infection: In rare cases, head trauma or illness can trigger narcolepsy.
How Narcolepsy Impacts Daily Life
 Narcolepsy isn’t just about feeling sleepy — it affects nearly every aspect of life. Common challenges include:
Narcolepsy isn’t just about feeling sleepy — it affects nearly every aspect of life. Common challenges include:
Struggles with work or school performance.
Safety concerns (e.g., falling asleep while driving).
Emotional stress, embarrassment, or social withdrawal.
Increased risk of depression and anxiety.
Diagnosis: How Doctors Detect Narcolepsy
If you suspect narcolepsy, a sleep specialist may order:
Polysomnography (Overnight Sleep Study): Tracks brain waves, heart rate, breathing, and muscle activity.
Multiple Sleep Latency Test (MSLT): Measures how quickly you fall asleep during the day and whether you enter REM sleep too soon.
Blood or spinal fluid tests: To check for hypocretin levels (in some cases).
Treatment Options for Narcolepsy
While there’s no cure yet, treatment can greatly improve symptoms and quality of life. Options include:
Medications
Stimulants: Such as modafinil or amphetamines to promote wakefulness.
Sodium oxybate: Helps manage cataplexy and improve nighttime sleep.
Antidepressants: May reduce cataplexy, hallucinations, and sleep paralysis.
Lifestyle & Behavioral Strategies
Scheduled naps: Short, planned naps throughout the day can help reduce sudden sleep attacks.
Consistent sleep routine: Going to bed and waking up at the same time daily.
Avoiding alcohol and sedatives: These worsen sleepiness and disrupt REM cycles.
Exercise & diet: Regular movement and balanced meals help regulate energy.
Practical Tips for Living With Narcolepsy
Here are steps you can try starting today:
Create a sleep-friendly bedroom (dark, cool, and quiet).
Break up long tasks with movement breaks or naps.
Inform friends, family, and coworkers so they understand your condition.
Consider safety adjustments (avoid long drives, operate machinery cautiously).
Use reminders, alarms, and planners to stay on track during bouts of fatigue.
When to See a Doctor
 You should seek medical advice if:
You should seek medical advice if:
You feel excessively tired most days despite adequate sleep.
You’ve experienced sudden muscle weakness with strong emotions.
You’ve fallen asleep at unsafe times (while driving, eating, or working).
Early diagnosis can help prevent accidents, improve functioning, and lead to effective treatment.
Conclusion: Hope and Better Sleep Are Possible
Narcolepsy may sound overwhelming, but you’re not alone — and you’re not powerless. With the right diagnosis, treatment plan, and lifestyle adjustments, many people with narcolepsy live full, active lives.
Daytime sleepiness doesn’t have to define you. By recognizing the symptoms, seeking medical care, and taking proactive steps, you can regain control over your days and nights.
Sleep may feel like a mystery at times, but with narcolepsy, knowledge is your strongest ally.